The Next Wave of Manufacturing: Human Organs
If manufacturing is a manifestation of creativity, then the gold at the end of the rainbow may be the ability to manufacture that which sustains human beings -- their organs.
While growing cells has been feasible for years, what has not been possible until now is the ability to actually produce tissue that in turn becomes a fully functioning organ.
See Also: Manufacturing Industry Technology News & Trends
But technology has advanced to such a level, through the use of 3-D printing, that scientists, and now companies, can layer cells on a bioprinter and produce tissue. The tissue will eventually be turned into implantable full-scale human organs.
"The ability to manufacture living human tissue for medical research and clinical practice has the potential to reshape the future of medicine," said Keith Murphy, CEO at Organovo, a San Diego-based company that designs functional human tissues.
And the need is great: Every 30 seconds a patient who could have been saved with tissue replacement dies.
"The power to deliver human tissue for transplant can help us impact even more patients, hopefully one day including those on organ transplant lists," said Murphy.
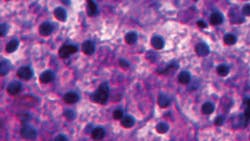
So how did scientists discover they could manufacture living tissue? One of the first discoveries was by Doris Taylor, who was the director of the University of Minnesota's Center for Cardiovascular Repair. In 2008, Taylor's research team was able to strip organs of their cellular make-up, leaving a decellularized "scaffold." The organs, such as heart, kidney, pancreas, lung and liver, could then be reseeded with cells that, when supplied with blood and oxygen, regenerate the scaffold into a functioning organ.
Moving from the lab to commercialization of this decellularization technology was achieved when Miromatrix Medical Inc. of Eden Prairie, Minn., received an exclusive global technology license with the University of Minnesota based on Taylor's research and became operational in 2010.
In deciding what to bring to market first, Robert Cohen, CEO of Miromatrix, explained that the decision to create Miromatrix Biomesh, a cardiac-derived biomesh, involved both the size of the potential market ($2 billion and growing) as well as the willingness of clinicians to use new and improved products.
"We also considered the benefit to our shareholders of a rapid entry into the commercial marketplace due to a 510(k) review pathway at the FDA," Cohen said. The product is expected to come to market within the next two years.
Cohen also said the relative ease of manufacturing was important. The company built its own plant to manufacture the product.
"We believe that our technology eventually will enable the replacement of entire organs harvested from donors, stripped of their cells and either transplanted as a biomesh or recellularized from the recipient or compatible cell lines," said Cohen.
Market Potential
Regenerative medicine is the name that has been given to this process of creating living, functional tissues to repair or replace tissue or organ function lost due to damage or birth defects -- and the potential market for it is sizable.
See Also: Regenerative Medicine -- Expanding Medical Manufacturing
"When incorporated into clinical practice, regenerative therapies may save $250 billion per year in the U.S. alone," said Gil Van Bokkelen, CEO of Athersys, at the Biotech Showcase 2012 workshop. His company, headquartered in Cleveland, Ohio, is developing a stem cell product for the treatment of multiple distinct diseases and conditions in the cardiovascular, neurological, inflammatory and immune disease areas.
The viability of this market has not gone unnoticed by the large pharmaceutical and medical device companies. Johnson & Johnson (IW 500/19) invested money in Miromatrix to assist with product development, and Pfizer (IW 500/17) has partnered with Athersys on its stem cell product.
Manufacturing a product based on decellularization required breakthrough technology. Organovo discovered that technology. The company was able to manufacture functional human tissues using 3-D bioprinting technology.
Here's how it works: Once a target tissue has been identified, the first step is to develop the bioprocess protocols required to generate the multicellular building blocks -- also called bio-ink -- from the cells that will be used to build the target tissue. The bio-ink building blocks are then dispensed from a bioprinter, using a layer-by-layer approach that is scaled for the target output. Bio-inert hydrogel components may be utilized as supports, as tissues are built up vertically to achieve three-dimensionality, or as fillers to create channels or void spaces within tissues to mimic features of native tissue.
Organovo's first release of a living human tissue for use in the in-vitro segment for drug discovery and medical research will be its liver model launch in 2014, Murphy told IndustryWeek. "We expect to add other tissue models regularly based on our completed strategic prioritization for the segment," he said.
Organovo said it is too early to predict when it might see a first engineered tissue therapy, as significant science and discovery remains to develop a tissue therapy, ensure safety and efficacy through controlled clinical trials and gain regulatory clearance as a medical device.
"Supplemental tissue therapies that could come in the form of tubes, patches or organoids are a developmental possibility today," Murphy said. "Larger replacement tissues remains a future goal. However, the insight gained through the development of supplemental tissue therapies can serve as key guideposts for the ultimate development of functional organ replacements."
With regard to the manufacturing process, Murphy said Organovo is in the early stages of defining its industrial strategy and is not restricted to any one approach.
"Certain constraints, such as the fact that living tissue products will be perishable and require specific handling, need to be included in our manufacturing decisions," he said.
Organovo expects to build tissues for the in-vitro segment in its own facilities for distribution using the systems already in place to handle medical and life science products of this type.
Collaboration for Quicker Time to Market
"Our proprietary technology is of great interest to a host of regenerative medicine experts at leading universities," Murphy explains. "Many of these experts have been working with the technology since the publication of the first journal article describing its invention and value. Rather than reinvent the wheel, we have chosen to work with the best among these experts on a product-by-product basis, rather than accomplish all of our product development purely internally."
There is no lack of research available. At the Wake Forest Institute for Regenerative Medicine in North Carolina, Dr. Anthony Atala created bladders that have been placed in seven patients and are still working. Engineers at Cornell University used 3-D printing techniques to build a new external human ear. And research is going on across the globe using bioprinting to develop other organs.
Deciding what to manufacture and when is yet another complication in this new field. Because our technology is new, as opposed to mature and well characterized, we spend considerable time up front assessing the probability of success with our potential partners to ensure we have confidence in the ability of the technology and advancements we may make with the technology to deliver, and we have a concise and well understood risk profile shared by the partners," said Murphy.
But hope abounds in this field. Miromatrix points out that 28,000 people die each year from chronic liver disease. Each year 17,000 people wait for 6,500 livers. "We can change that," the company says.